Introduction
There
is much value in having a common language to talk about healthcare amongst
different stakeholders. The common language should be easy to understand yet
accurate. The common language within the healthcare delivery system of Abu
Dhabi is defined in the data dictionary. All communications with HAAD need to
use the common language defined in the data dictionary. Any electronic
transactions between ePartners
need to be mappable with the data dictionary. The
data dictionary defines key concepts, such as a Person, as well as associated elements, e.g., Patient.FirstName
and describes the relationships between concepts and elements.
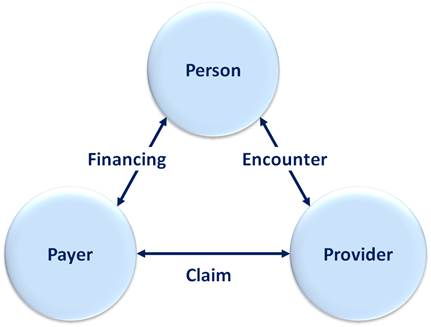
Key concepts
Healthcare
systems help individual Persons
obtain better health. A person can be a Patient who has an Encounter with a Provider.
The Provider then claims some or all of the charges from the Payer. The payer in turn collects insurance
premiums (Financing) from its
members, who are individual persons. The relationship between these key
concepts is shown below.
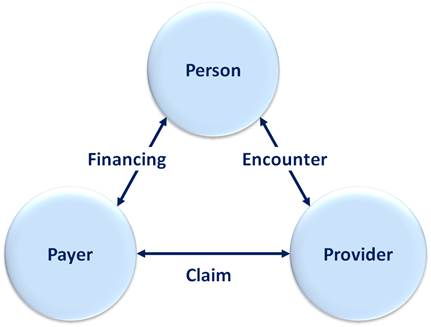
When a patient has an encounter with a provider,
the provider needs to know what was done with the patient – an Activity such as
a lab test – to be able to charge for it. Activities may or may not lead to an
Observation, such as the result of a lab test. The Activity and Observation
concepts are both depicted in the Figure below, together with a summary of all
the data elements within each concept.
Key concepts
and selected associated elements

Encounter
An Encounter starts
when a Patient is first brought under the care of a responsible healthcare
professional and ends when the Patient stops being under the care of a
responsible healthcare professional at the healthcare provider.
Example 1 | A
Patient has an accident at home and is driven by his family to the emergency
room of a local hospital. After triage in the emergency room, the Patient is
admitted to a ward and has surgery a few hours later. After five days the
Patient is discharged home. The time period from being registered in the
emergency room until discharge from the hospital is considered to be one
Encounter.
Example 2 | A
Patient has an out-patient consultation during which she undergoes a lab test
and receives a prescription, which she collects on her way out of the hospital.
Four days later she has an x-ray, and a further two days later a follow-up
appointment with a doctor. The Patient has had three Encounters:
outpatient consultation + lab test + prescription
X-ray
follow-up appointment
Example 3 | A
Patient has an outpatient consultation, during which he receives a lab test,
does an x-ray and receives a prescription, which he collects on the way out of
the hospital. This Patient has only one Encounter: out-patient consultation +
lab test + x-ray + prescription
Claim
A claim is an
original request for payment for health services provided to a single Patient.
Claims are generally linked to Patients who are covered by health insurance.
For the purposes of this guidance, any invoices made out to non-insured
Patients should also be considered as Claims.
Activity
A Claim may comprise one or many Claim items, often
referred to as service lines. Analogously, an Encounter may comprise one or
more items, e.g., only a visit to the emergency room (one item), or for
example, a visit to the emergency room followed by an admission, lab test,
diagnostics and prescriptions (five items).
An Activity is any Claim item or Encounter item.
Generally a Claim item corresponds to an Encounter item, so
every Claim item/Activity item is considered an Activity. This could be the
case for example for a first outpatient consultation or a prescription, two
separate activities.
Some Encounter items however do not correspond with Claim
items. For instance, individual surgical procedures are Encounter items, yet
they may be claimed summarily as a DRG or flat fee (the Claim item). Both the
surgical procedures as well as the DRG or flat fee are considered individual
activities.
Some Claim items don’t have corresponding Encounter items. In
the example above, the DRG Claim item is a Claim item, but not an Encounter
item.
Example | A Patient has elective surgery and receives a
tailored drug cocktail, which is not covered by his primary insurance. For this
one Encounter the hospital makes two Claims: one to the primary insurance which
is billed as a DRG, and one to the supplementary insurance for the expensive
drugs. The two Claims need to be reported in two separate records. The
Encounter information on each record should include information on the
procedures performed, even if they are not charged. On the first Claim the only
charge relates to the DRG; on the second, the only charge relates to the drugs.
Each record should specify those chargeable activities
which are related to the Claim.
Example | A Patient has an outpatient consultation and
receives a prescription. If the provider makes two separate Claims for this one
Encounter, this would result in two records, one covering the consultation and
one covering the prescription. The record claiming the consultation would only
have the consultation Activity, while the record claiming for the prescription
would only comprise the prescription Activity.
Observation
An Observation is the result of an Encounter Activity such
as a diagnostic test, lab work, etc. An Activity may have multiple
Observations, but an Observation can only be the result of one Activity. In the
simplest form for example, a blood pressure test (the Activity) results in a
blood pressure reading (the Observation).
Laboratory
observations, also known as findings, are essential analytical data elements
for disease management, outcome analysis and other studies.